As flu, RSV, and COVID-19 continue to surge this winter, many people wake up feeling miserable and face a familiar question: Where should I go for care—and what can I safely take to feel better?
Health systems say knowing both answers matters more than ever. Emergency rooms are crowded, and at the same time, poison control centers are seeing a spike in medication mistakes tied to common cold and flu remedies.
When the ER isn’t the right first stop
Doctors say most people with mild respiratory illness don’t need emergency care. Fever, cough, congestion, and body aches can usually be managed at home or through a primary care doctor, urgent care clinic, or virtual visit—especially if you can breathe comfortably and keep fluids down.
“If your symptoms are mild—like a fever under 103 degrees and no trouble breathing—there’s no real reason to go to the emergency room,” said Dr. Shawn Phillips, a family medicine physician with Penn State Health.
Emergency departments prioritize the sickest patients first. That means long waits for non-urgent cases and more exposure to other illnesses in crowded waiting rooms.
Doctors say the ER is the right choice if someone can’t breathe, can’t stay hydrated, develops chest pain, confusion, seizures, or if chronic conditions suddenly worsen. Older adults with lung disease or weakened immune systems are at higher risk for complications and should seek care sooner.
Guidance from the Centers for Disease Control and Prevention also urges adults 65 and older, young children, pregnant people, and those with compromised immunity to contact a provider early if flu symptoms appear.
Acetaminophen: the hidden risk in your medicine cabinet?
While deciding where to get care is one challenge, what people take at home is becoming another. Since November 2025, the New Jersey Poison Control Center has managed dozens of cases involving accidental overdoses of acetaminophen—the active ingredient in Tylenol and hundreds of cold and flu products.
“Cold and flu season is the time of year when we see an uptick in calls related to overuse of acetaminophen,” said Diane Calello, executive and medical director of the center at Rutgers New Jersey Medical School.
Why acetaminophen overdoses happen so easily
Many people don’t realize they’re taking the same drug more than once—just under different brand names.
Acetaminophen is the active ingredient in Tylenol, but it’s also hidden inside hundreds of cold, flu, pain, and sleep products. In fact, there are 600+ medications on the market that contain it.
That’s how “doubling up” happens.
You might take:
- A pain reliever for body aches
- A cough or cold medicine for congestion
- A nighttime formula to help you sleep
All three can contain acetaminophen.
Taken together—or too close in time—you can accidentally exceed the safe daily limit, even if you’re following each label correctly.
Common products that often contain acetaminophen include:
- Multi-symptom cold and flu formulas
- Fever reducers
- Headache and migraine medicines
- Nighttime “PM” pain relievers
- Some prescription pain medications
Why this matters:
Too much acetaminophen can cause serious liver damage, and symptoms may not appear right away.
A simple safety check:
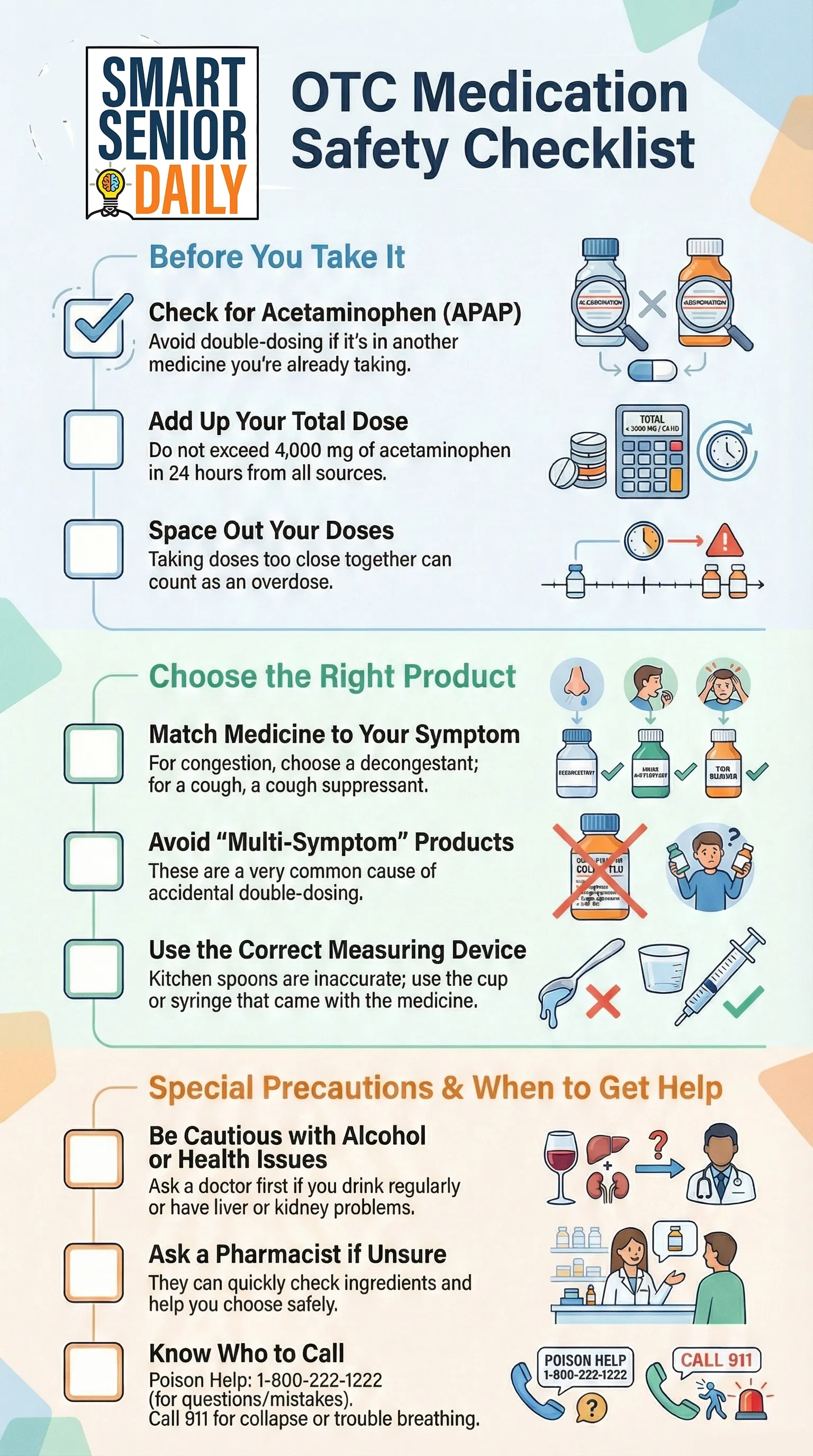
Before taking another medicine, look at the “Active ingredients” line on the label. If you see acetaminophen, count it toward your daily total—and don’t stack it with another product that contains the same ingredient.
When in doubt, pharmacists and poison control specialists can help you sort it out quickly.
The most common mistakes...
... are taking doses too close together or unknowingly combining multiple products that all contain acetaminophen. With more than 600 medications on the market using the same ingredient, doubling—or tripling up—can happen fast.
Health experts warn that exceeding the daily maximum of 4,000 milligrams from all sources combined can lead to severe liver damage, kidney failure, or worse. Children are at even higher risk because much smaller amounts can cause harm.
What to take instead of stacking acetaminophen
If you’re already taking a medicine that contains acetaminophen, you still have options to treat symptoms—without doubling up.
For congestion or a stuffy nose
- Use a saline nasal spray or rinse
- Try a humidifier or steamy shower
- Choose a decongestant-only product (no pain reliever included)
For cough
- Look for a cough suppressant or expectorant by itself
(Check labels to be sure acetaminophen is not included) - Honey or warm fluids can help soothe irritation
For fever or body aches (if acetaminophen is already on board)
- Ibuprofen may be an option for some adults
(Not recommended if you have kidney disease, stomach ulcers, or are advised to avoid NSAIDs—check with your doctor or pharmacist) - Non-drug options like rest, fluids, and cool compresses still help
For sleep
- Avoid “PM” pain relievers unless you’ve checked the ingredients
- Try non-medication sleep supports:
- Consistent bedtime routine
- Dark, cool room
- Herbal teas (like chamomile)
A smart rule of thumb
Treat one symptom at a time, using the fewest ingredients possible. Multi-symptom products are convenient—but they’re the most common cause of accidental acetaminophen overdose.
If you’re unsure, ask a pharmacist or call Poison Help at 1-800-222-1222. It’s free, confidential, and available 24/7.
Here's a guide you can print out and keep handy when mixing OTC medications:
Safer ways to recover at home
If symptoms are mild, supportive care is usually enough:
- Rest and drink fluids
- Use a humidifier for congestion
- Take only symptom-specific medicines
- Read labels carefully before combining products
- Test for flu or COVID-19 if symptoms fit
If a test is positive, a doctor may prescribe antiviral medications, which work best when started within 48 hours.
Flu shots can still help, even late in the season. Vaccination reduces the risk of severe illness and hospitalization, especially for older adults.
When in doubt, ask
Doctors stress that choosing the right care setting—and using medications safely—helps protect both patients and strained health systems. For medication questions, poison control specialists are available 24/7 at 1-800-222-1222. Emergencies like trouble breathing, seizures, or collapse still warrant a call to 911.
The takeaway: most winter illnesses can be managed without the ER, but small decisions—like mixing cold medicines—can turn a rough week into a medical emergency.
Disclaimer: This article is for general informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician, pharmacist, or other qualified health provider with any questions you may have about a medical condition or medications. In an emergency, call 911 immediately.