Part 2: Preparing for Diagnosis, Testing & Talking to Doctors
The moment the word Alzheimer’s enters the conversation, everything speeds up.
Adult children often arrive at this stage carrying dread, urgency, and the sense that they should already know what to do. Doctor appointments suddenly feel loaded. Every forgotten word feels ominous. Every delay feels risky.
This stage isn’t about rushing toward a diagnosis. It’s about slowing down just enough to gather clarity—while your parent can still participate in the process.
What medical evaluations actually matter
Preparing for testing can feel overwhelming, especially when emotions are already running high. April McKenna, a Certified Dementia Practitioner at Agemark Senior Living who trains senior living teams nationwide, says many families don’t realize how often dementia-like symptoms turn out to have other explanations.
“There are conditions that can be mistaken for dementia—depression, infections such as UTIs, medication side effects, and much more,” McKenna explains. “You want to ensure your loved one’s condition isn’t something treatable. Getting an accurate diagnosis is a vital step.”
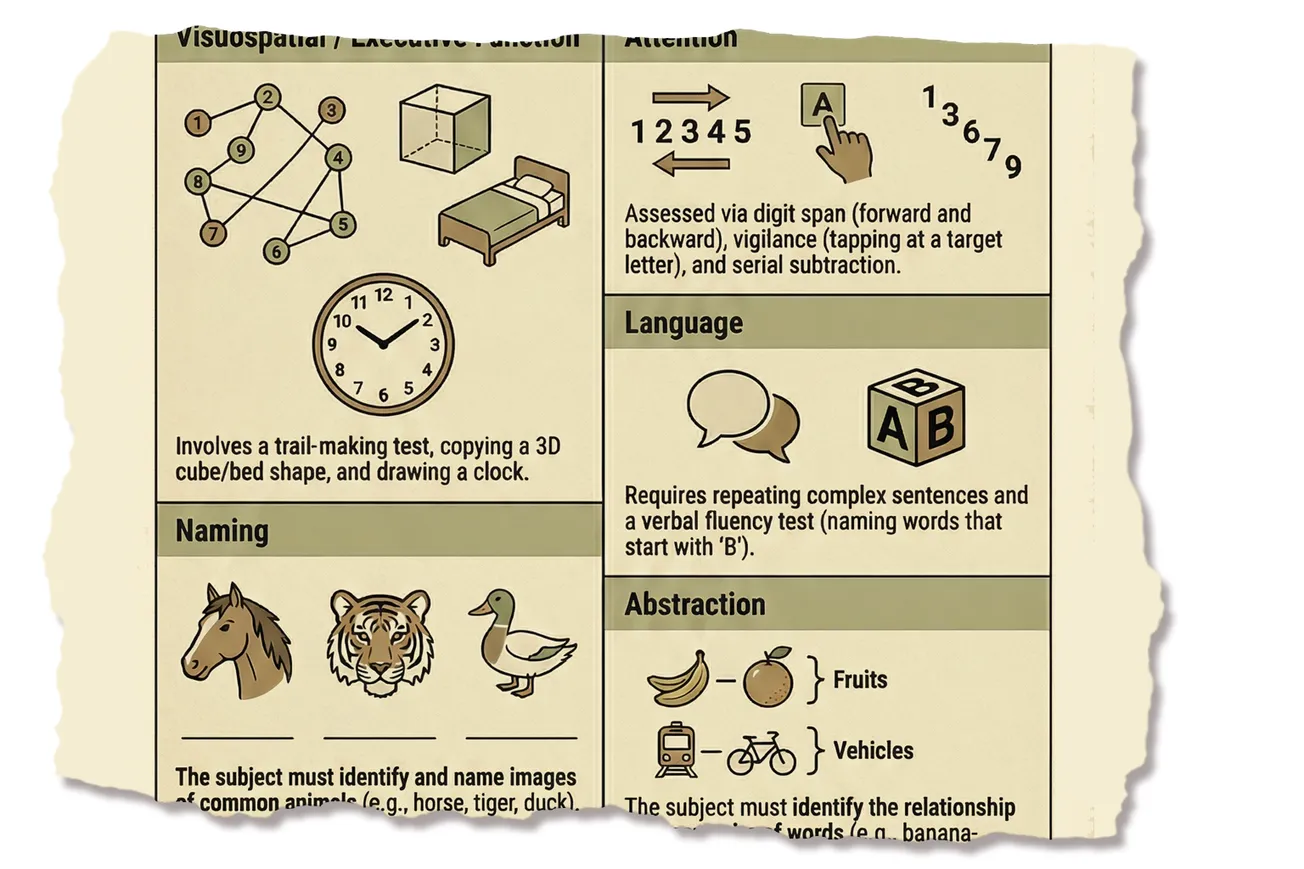
That’s why a thorough evaluation usually involves several components—cognitive testing, medication review, lab work, and sometimes brain imaging. The goal isn’t to label your parent prematurely. It’s to rule out reversible causes before assumptions are made.
An accurate diagnosis doesn’t erase fear—but it replaces uncertainty with information.

Advocating without taking over
Once testing begins, many adult children feel pressure to step in forcefully. Nicole Brackett, an LPN and Director of Quality and Care Delivery at Homewatch Caregivers with more than 30 years in dementia care, cautions against that instinct.
“Advocacy does not mean taking over—it means ensuring your parent’s voice is heard,” Brackett says. “Even with an Alzheimer’s diagnosis, many individuals can still express preferences and make decisions about their care.”
She encourages adult children to ask open-ended questions—What feels most comfortable? How would you like this handled?—rather than assuming decision-making authority. Framing your role as support instead of control helps preserve dignity and reduces feelings of helplessness.
Read Nicole Brackett's full comments on on what adult children need to know before fear takes over
One of the most important things adult children can do is to respect their parents’ autonomy. Even with an Alzheimer’s diagnosis, many individuals can still express preferences and make decisions about their care.
It is important to encourage them to participate in conversations about treatment, daily routines, and living arrangements. Ask open-ended questions like, ‘What feels most comfortable for you?’ or ‘How would you like this handled?’
This approach helps maintain dignity and a sense of control, which is critical for emotional well-being."
Advocacy does not mean taking over—it means ensuring your parent’s voice is heard. When speaking with healthcare providers, frame your role as a supporter rather than a decision-maker.
For example, you might say, ‘My parent would like to…’ or ‘They’ve expressed that…’; this reinforces that the individual remains central in their care decisions. Empowering them to stay involved, even in small choices like meal preferences or activity planning, preserves independence and reduces feelings of helplessness.
How to show up at doctor appointments
Going to appointments together is important, but how you show up matters. Stephanie Leanes, Director of Caregiver Support at Lutheran Home & Harwood Place, says appointments can be intimidating for someone already struggling with memory or language.
“Let them speak first in appointments and step in when clarification is needed,” Leanes advises. “Never talk about them as if they are not in the room—even in progressed stages.”
Writing questions down ahead of time helps both parent and adult child stay grounded. Explaining your presence as support—not supervision—can lower anxiety and prevent the visit from feeling adversarial.
Read Stephanie Leanes' full comments on what adult children need to know before fear takes over
New Dementia Diagnosis, New Reality.
Now What?Hearing your loved one has dementia can throw us into a state of shock, disbelief, fear, anger, grief, loss and occasionally relief. There is finally a reason for their behavior, and they are not doing it to irritate you.
Should you jump into action to figure out what the next steps are? There are so many emotions to process that some time should be taken to absorb the impact of what you have just been told. Processing doesn’t change the diagnosis, but it changes how someone lives with it.
Have those important conversations about what the person diagnosed wants you to know and what they want for the future before they can no longer tell you. Move forward with clarity instead of panic.
When someone you love receives a dementia diagnosis, many of us feel a mix of fear, urgency and protectiveness. Effective advocacy doesn’t mean we take over control. It means we listen. It means empowering your loved one and protecting their dignity for as long as possible.
Offer choices throughout the entire journey. Those choices and types of decisions will change over time as dementia progresses, but we need to make it a priority to NEVER forget this. Empower them, don’t strip them of their confidence.
Going to doctor appointments with your loved one with dementia is vital to receiving information firsthand rather than depending on them to remember everything that was discussed.
It can be a daunting task for them and cause frustration. Instead, explain to them that you want to be there to support them in every way possible. Let them speak first in appointments and step in when clarification is needed.
You both will have questions in the beginning. Write them down and bring with you or send a message to the doctor before the appointment. Never talk about them as if they are not in the room, even in progressed stages.
Empowering people with dementia means avoiding unnecessary correction. This is a disease of loss, and we need to protect their dignity. In later stages of the disease, we need to live in their world because not doing so is only going to break down the relationship.
Read up on what therapeutic fibbing is. It is a game changer if you continue to correct them. Choose connection over perfection. Education about this disease is your responsibility and it will improve the quality of their life as well as yours.
In the end, the goal is to walk alongside them with compassion and respect so their voice remains present for as long as possible. This will allow more moments of joy!
Asking the right questions early
At this stage, families often focus solely on what’s wrong. That’s natural—but incomplete.
Along with questions about testing and diagnosis, it’s important to ask what changes to expect next, what warning signs matter most, and how to approach difficult topics like driving, finances, and medications before a crisis forces those conversations.
McKenna emphasizes that timing makes a real difference. “The most important step is acting before an emergency forces decisions to be made,” she says. “Early conversations, even when uncomfortable, give families more options and clearer guidance.”
Read April McKenna's full comments on on what adult children need to know before fear takes over
What medical evaluations matter
Preparing for a possible diagnosis can feel overwhelming, especially when emotions and uncertainty run high. Knowing what to expect and how to show up can make this stage far less intimidating.
Not all medical evaluations are created equal.
A thorough assessment often includes cognitive testing, medication reviews, lab work, and brain imaging when appropriate. These steps help rule out reversible causes and establish a clearer picture before assumptions are made.
There are conditions that can be mistaken for dementia - depression, infections such as UTI's, medication side effects, and much more. You want to ensure your loved one's condition isn't something treatable. Getting an accurate diagnosis is a vital step.
How to advocate without taking over
Advocating for a parent doesn’t mean speaking over them. The goal is to support - not replace - their voice. Sharing observations respectfully, asking questions, and inviting your parent into the conversation helps maintain trust and dignity throughout the process.
Questions to ask doctorsHow to discuss driving, finances, medication, independence
What to do before a crisis happens
The most important step is acting before an emergency (such as a car accident, getting lost, a physical health incident, etc.) forces decisions to be made. Early conversations, even when uncomfortable, give families more options, clearer guidance, and a stronger foundation for what comes next.
Why timing matters more than certainty
Many families delay action because they’re afraid of being wrong—afraid of overreacting, afraid of opening a door they can’t close.
But waiting for certainty often means decisions get made during chaos: after a fall, a car accident, or a frightening episode of confusion. Acting earlier doesn’t mean jumping to conclusions. It means building a foundation while your parent can still help shape what comes next.
This stage isn’t about fixing everything.
It’s about replacing panic with preparation—and making sure your parent’s voice stays present for as long as possible.
FAQ: What Readers Ask Most Often
Questions That Readers Frequently Ask
How do I know when it’s time to get my parent tested?
Testing is worth pursuing when changes are becoming consistent, not occasional. If memory issues, confusion, or behavior changes are happening more often, lasting longer, or starting to affect daily life—like managing medications, finances, or driving—it’s time to talk with a healthcare professional. You don’t need certainty. You need patterns.
What if it turns out not to be Alzheimer’s?
That’s actually common—and good news. Conditions such as depression, sleep disorders, infections, vitamin deficiencies, or medication side effects can mimic dementia symptoms. A thorough evaluation helps rule out treatable causes before assuming a progressive disease.
Should adult children always attend doctor appointments?
Yes, when possible. Many parents feel overwhelmed trying to remember symptoms, timelines, and medical details. Attending appointments helps ensure accurate information is shared and reduces stress—but your role should be supportive, not dominant.
How do I advocate without embarrassing or upsetting my parent?
Let your parent speak first. Step in only to clarify or add observations. Avoid correcting them in front of the doctor or talking about them as if they aren’t present. Framing concerns as shared observations—“This is something we’ve both noticed”—helps preserve dignity.
What questions should I ask the doctor at this stage?
Focus on clarity, not conclusions. Ask what tests are recommended and why, what conditions are being ruled out, what changes to watch for next, and how to handle sensitive topics like driving, medications, or finances before a crisis occurs.
What if my parent refuses testing?
Avoid arguing. Resistance is often rooted in fear. Emphasize that testing is about overall health and ruling out reversible issues—not labeling or taking away independence. Sometimes approaching it as a routine checkup or medication review lowers defensiveness.
Is it better to wait until symptoms get worse?
Usually, no. Waiting often means decisions are made during emergencies, when options are limited and emotions are high. Early conversations—even uncomfortable ones—give families more choices and allow parents to participate in planning.
What’s the biggest mistake families make at this stage?
Rushing—or freezing. Some families push too hard too fast. Others wait too long out of fear. The healthiest approach is steady, informed, and respectful: gather information, keep communication open, and move forward together.
Medical & Educational Disclaimer: This article is for educational and informational purposes only and is not intended to provide medical advice, diagnosis, or treatment. Alzheimer’s disease and other forms of dementia can present differently from person to person, and only a qualified healthcare professional can evaluate symptoms, order appropriate tests, and make a diagnosis.
If you have concerns about memory, behavior, or cognitive changes — whether for yourself or a loved one — speak with a physician, neurologist, or other qualified medical provider promptly. Early evaluation can help identify treatable conditions, clarify next steps, and provide access to appropriate support and resources.
Smart Senior Daily does not replace professional medical guidance. Always consult a healthcare professional with questions about health conditions or care decisions.